by Heather Lasseter, PhD, Medical Writer
The high-profile deaths of actors Heath Ledger and Philip Seymour Hoffman have brought the stark reality of prescription and illegal drug abuse into the public eye. The loss of Heath Ledger – who died from a fatal overdose of oxycodone, hydrocodone, and benzodiazepines – highlights the “opioid epidemic” that has been sweeping the United States. But the good news? Expanded availability and new formulations of drugs designed to combat drug overdose may help curb the growing number of opioid overdoses.
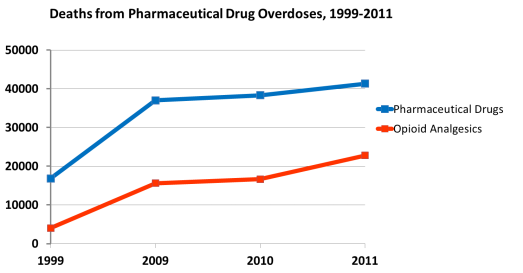
According to the Centers for Disease Control and Prevention (results published in the Journal of the American Medical Association), deaths from drug overdoses have increased steadily over the past two decades, with opioid drug use contributing heavily to these fatalities.
And the statistics surrounding drug overdose are staggering:
- 38,329 people died of drug overdose in 2010 – a more than 2-fold increase from 1999
- More than 100 people die from drug overdose every day in the US
- Drug overdose was the leading cause of death due to injury, surpassing motor vehicle accidents as a cause of death among 25- to 64-year-olds
Shockingly, the majority of overdose deaths in recent years involve pharmaceutical drugs. Of these, opioid analgesics like oxycodone, hydrocodone, and methadone played a prominent role: pharmaceutical opioids were involved in 74% of fatal drug overdoses, and they contributed to more fatalities in 2008 than the street drugs cocaine and heroin combined.* Aside from the tragic loss of life, the monetary costs of opioid abuse – including workplace, healthcare, and criminal justice costs – were more than $55 billion in 2007.
| *According to the 2012 National Survey on Drug Use and Health, over 2,000,000 individuals aged 12 and older were dependent on or had abused pain killers in the past year, compared to approximately 1,120,000 and 470,000 individuals who had used cocaine or heroin, respectively. |

Data from Jones CM, et al. JAMA. 2013;309(7):657-659. *Deaths are not mutually exclusive; deaths involving more than one drug or drug class are counted multiple times.
With sales of these pharmaceutical painkillers skyrocketing by 300% since 1999, a solution is clearly needed to turn the tide in opioid use that contributes to overdose deaths.
A medication that specifically combats opioid overdose exists, and has been used for years in medical settings. This drug, naloxone,* can reverse the fatal effects of opioids and, as part of emergency response kits distributed to heroin users and other opioid drug users, has been shown to reduce fatal overdoses.
| *Naloxone should not be confused with naltrexone, which is longer acting and used to treat alcohol and opioid dependence rather than acute drug overdose. |
So how does naloxone combat opioid overdoses?
Opioid agonists, like oxycodone or heroin, bind to opioid receptors located throughout the central and peripheral nervous systems as well as in the gastrointestinal tract. While their action leads to clinically beneficial effects such as analgesia, they can also produce feelings of euphoria (hence the abuse potential) and dangerous side effects including respiratory depression, decreased heart rate, loss of consciousness, and even coma. Naloxone works by rapidly reversing the underlying cause – not just the symptoms – of an opioid overdose. With an extremely high affinity for μ-opioid receptors, and as a competitive antagonist at these receptors, naloxone essentially floods the nervous system and knocks opioids out of the way. This results in a rapid reversal of overdose symptoms – giving the opioid user a “second chance.”

Crystal structure of the μ-opioid receptor bound to a morphinan antagonist, from WikimediaCommons by Metilisopropilisergamida.
Because naloxone undergoes high first-pass metabolism, oral ingestion of naloxone only affects receptors in the gastrointestinal tract. Hence, it must be delivered by intravenous, subcutaneous, or intramuscular injections, or via the nasal passages. However, first responders such as police officers have expressed reluctance to administer naloxone injections to overdose victims and are similarly hesitant to use naloxone nasal inhalants due to their off-label use. The availability of these medications has also been limited, especially in rural areas.
Enter the new prescription treatment Evzio™.
Evzio,a naloxone HCl injection, was fast-tracked to receive approval by the US Food and Drug Administration on April 3, 2014 – 2 months ahead of the planned approval date – and became available on July 10. So where does Evzio fit in? Unlike other naloxone treatments such as Narcan® (which can be used either as an injectable or inhalable agent), Evzio is the first FDA-approved naloxone injector that permits easy administration without training, similar to the EpiPen® used for treatment of anaphylaxis. Evzio rapidly delivers a single 0.4 mg dose of naloxone via a handheld auto-injector that administers either an intramuscular or subcutaneous injection. The device also provides visual and voice instructions for how to deliver the medication, and can be easily transported or stored. This puts the power to combat overdose firmly in the hands of friends and family – those most likely to be at the scene of an overdose.
Nevertheless, “rescue” treatments for drug overdose face steep criticisms – and potential barriers to implementation.
Detractors suggest that easy access to overdose treatments will provide opioid users with a false sense of security and encourage risky and/or illegal drug use, despite evidence that enrollment in naloxone and resuscitation programs produces a decline in drug use – at least among heroin users. Further, high costs associated with new treatments like Evzio may create a significant barrier to use. Speaking to the Boston Globe, drug policy researcher Leo Beletsky of Northeastern University estimated that Evzio may cost $200 per dose compared to $15-$40 for the nasal spray. (Kaléo, the manufacturer of Evzio, is offering a Patient Assistance and Payment program to enable more widespread access to the drug.)
Another salient point is that drugs like Evzio and Narcan do not preclude prompt emergency medical attention when an overdose is suspected. These medications only combat opioid overdose, not overdose of other medications like benzodiazepines, and their effects may not outlast those of the opioids, whose half-lives (typically multiple hours) are longer than that of naloxone (30-80 minutes). Thus, an individual may still be at risk of dying after receiving initial treatment, necessitating repeated dosing and additional medical care.
That said, drug overdose prevention programs are a powerful force for combating the rising tide of opioid-induced deaths. For instance, Project Lazarus, North Carolina’s Wilkes County overdose prevention program, has been advocating the use of naloxone to reverse opioid toxicity and has developed other educational tools for emergency department and primary care physicians. The result? The county, which had the third highest rate of drug overdoses in the nation, has seen a progressive, 28-month drop in overdose deaths for a 69% reduction in just over 2 years. Officials hope this program may be spread across the state and serve as a model for programs nationwide.
It is possible to deliver pain relief without a heavy overdose risk – and opioids remain a powerful part of our arsenal for treating acute and chronic pain such that removing access would be unethical for those in genuine need. But as stated by the FDA, “opioids are powerful medications that can help manage pain when prescribed for the right condition and when used properly. But when prescribed by physicians to patients who should not receive them, or when used improperly or for recreational purposes, they can cause serious harm, including overdose and death.”
| For more information on deaths related to pharmaceutical drug and opioid overdose, please visit the CDC webpages: |
| www.cdc.gov/homeandrecreationalsafety/overdose/facts.html |
| www.cdc.gov/media/releases/2013/p0220_drug_overdose_deaths.html |