By Anna Lau, PhD, Medical Writer
Chronic diseases (eg, asthma, diabetes, hypertension) are persistent conditions that can be controlled but not cured. Without treatment, chronic diseases increase the risk of death, but with treatment, patients can enjoy fairly normal lives. Yet getting patients to take their medications as directed (adhere to a treatment plan) is a widespread problem. For example, direct costs of nonadherence to treatments for diabetes, hypertension, and hypercholesterolemia together exceed $105 billion annually in the US. It’s estimated that only 50% of patients with chronic conditions are adherent to treatment. What gives?
Can game theory shed light on poor adherence to chronic medication?
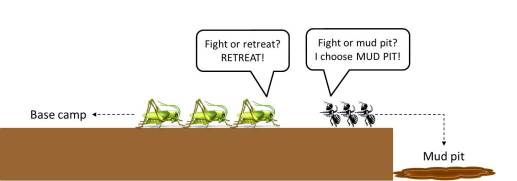
Game theory is the study of strategic decision-making. The prisoner’s dilemma is a well-known game of strategy that explores how two parties balance cooperation and competition in decision-making. Game theory has also been used to understand how decisions are made in conflict situations. By drawing an analogy to fighting a battle, let’s see what we might learn by applying conflict strategy to coping with a chronic disease. In his book The Strategy of Conflict (1960), Thomas Schelling suggests potential advantages to limiting one’s own options in a conflict situation. For example, in a hypothetical battle between grasshoppers and ants, a savvy ant general who positions its army at the edge of a cliff is more likely to win (Figure 1). Given the choice between certain death and fighting, the army ants are more likely to fight (and fight hard!).
| The opposing grasshopper army is unlikely to charge forward and attack, because doing so would assure mutual destruction. |
But what if the choice were between fighting and something less than certain death (Figure 2)? Would the army ants fight as hard? Probably not.
Patients who experience acute illnesses of sudden onset and short course, such as heart attacks, may experience severe symptoms. And on average, about 15% of heart attacks are fatal. It’s hard to imagine that a patient in the midst of a heart attack would willfully refuse treatment. Given the choice between possible death and accepting treatment, patients are highly motivated to literally fight for their lives.
But patients with chronic conditions may not feel sick or experience overt symptoms most of the time. The motivation to faithfully take medications may be diminished, because the choice for them is between bearing the burden of chronic medication or living with an asymptomatic (or mildly symptomatic) condition. And if the medication causes side effects, or is painful to administer (like injections), inconvenient to take, or expensive, the choice may be easier. In addition, if effective rescue therapies are available, the motivation to adhere to chronic medication may be even lower. Patients might choose to take rescue medications occasionally over chronic medications daily.
Okay, now what about decision theory?
Decision theory explores factors that go into decision-making. It’s related to game theory, except that it focuses on how individuals, not multiple parties, make decisions. In their paper Choices, Values, and Frames (1984), Kahneman and Tversky describe loss aversion, the observation that people dislike losing something more than they like gaining something. For instance, Kahneman recounts asking students in his class to gamble on a coin toss. Given the condition that they would lose $10 if the coin toss turned up tails, how much money would they insist on winning in order to agree to gamble? The answer was usually more than $20. Loss aversion stems from the endowment effect, the tendency of people to value something more once they own it. For instance, if you ask home sellers and buyers to estimate the value that the other party would put on a home for sale, sellers tend to overestimate the value and buyers tend to underestimate. Loss aversion often leads to status quo bias, the preference of people to do nothing instead of making a change. In a set of experiments, people were more willing to accept an electric shock than take the chance of reducing that shock by pressing a button.
Asymptomatic patients may not be willing to change their current lifestyles to take chronic medications, even if the potential payoff is better health or delayed disease progression. This phenomenon has been termed “patient inertia.” Researchers believe that nonadherence to treatment may have less to do with lack of understanding of drug benefits and more to do with this tendency to do nothing (maintain the status quo).
Certainly there are other barriers to adherence…?
Of course, and those barriers include provider-related factors (eg, prescribing an overly complex regimen, failure to communicate effectively with the patient), patient-related factors (eg, poor understanding of disease or benefits/risks of treatment), and healthcare system–related factors (eg, access to insurance coverage or to medication). These factors affecting treatment adherence are better studied than factors related to game theory or decision theory. Given how applicable game theory and decision theory are in explaining economic behaviors, it may be worthwhile to further investigate their potential role in treatment adherence.
As the term “inertia” implies, patients can be coaxed to adopt new behaviors such as taking daily medication by making those behaviors routine, easier, and more accessible. For example, tie the act of pill-taking to a daily event, such as eating breakfast or brushing teeth. Prescribe preloaded syringes to eliminate a step in treatment administration. And (if safe) leave medicine bottles in easy reach instead of inside a medicine cabinet. These small changes in behavior can improve adherence and possibly save hundreds of millions of dollars or more each year in healthcare costs.